Hormones rejuvenate, regenerate and restore. They serve as powerful chemical messengers sent to specific cells throughout your body to orchestrate many of your body’s internal functions and how your organs behave. Even a small fluctuation in levels can cause big changes in cells or even disrupt the balance throughout your entire body. Too much or too little of a hormone can have serious consequences.
This is a key reason to be cautious when selecting hormone replacement therapy. The goal should always be hormonal balance and based in science rather than experimentation or guessing. Many therapies merely attempt to replenish estrogen and/or progesterone and testosterone but never achieve homeostasis. Too many physicians lack the expertise or knowledge to attain the proper outcome.
Any endocrinologist will tell you that hormonal balance equates to health. Research continues to indicate that hormones are key to the intricate interrelationships of the body’s parts and systems. They play a pivotal role in your overall health.
You can see why hormone fluctuation and depletion during perimenopause, menopause and andropause wreak havoc in the body. Research evidence repeatedly points to the relationship between the hormonal imbalance of menopause and andropause, and an increased risk for developing cancer, osteoporosis, stroke, thyroid malfunction and other age-related disorders.
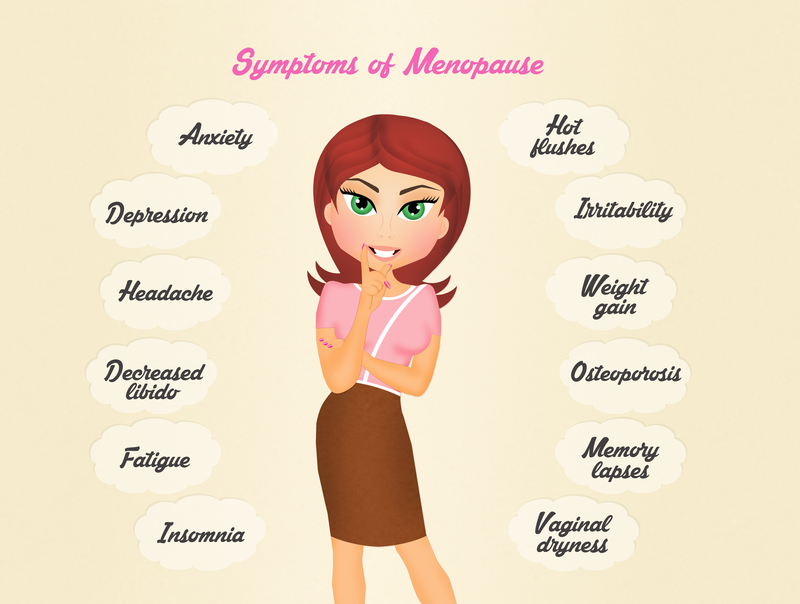
It is actually considered the norm for men and women to experience a decline in health at this stage of the aging process. You’re also more likely to experience problems like depression, anxiety, memory loss, hot flashes, sleep disturbances, libido issues, and sexual dysfunction, to name just a few.
Testosterone is a steroid hormone from the androgen group. It is formed from cholesterol in the body and primarily secreted in the testes in men and the ovaries in women, with a small amount secreted by the adrenal glands. The average adult male body produces about ten times more testosterone than an adult female body.
There is strong evidence that testosterone helps maintain optimum health in both men and women. It directly affects muscle development, fat levels, bone mass, many different parts of the brain including cognitive function, moods, depression, energy levels, ability to have orgasms, heart health and the ability to sleep, among other benefits.
For a man, testosterone is his most important hormone. It provides critical protection against osteoporosis, heart and prostate disease. Every man experiences a gradual decline in hormone production as he gets older. Beginning at age 30, his body starts to manufacture less and less testosterone, losing approximately one to three percent per year. Then, sometime between ages of 40 and 55, testosterone levels drop dramatically and signal the onset of andropause—the medical term for the male equivalent to menopause. When this happens, a man often finds himself lacking in sexual desire, gaining weight, losing muscle mass and feeling sluggish, depressed and irritable.
Research suggests that attention, memory, and spatial ability are important cognitive functions affected by testosterone. There’s even preliminary evidence linking low testosterone levels as a risk factor for cognitive decline and possibly for dementia of the Alzheimer’s type.
(HogervorstE, Bandelow S, Combrinck M, Smith AD (2004). “Low free testosterone is an independent risk factor for Alzheimer’s disease”. Exp. Gerontol. 39(11-12): 1633–9.)
According to one recent study, it is becoming increasingly evident that low testosterone levels in aging men are associated with increased mortality from coronary heart disease and other vascular disorders. It goes on to say that NATURAL, not synthetic, testosterone therapy has wide-ranging health benefits for these conditions while providing positive effects on problems such as obesity, metabolic syndrome, type 2 diabetes and erectile dysfunction.
Even so, testosterone deficiency in aging men continues to be an “under-treated condition” according to an article published online by the National Center for Biotechnology Information. It goes on to say that “Maintaining normal testosterone levels in elderly men has been shown to improve many parameters which are thought to reduce cardiovascular disease risk such as increased lean body mass, decreased visceral fat mass, decreased total cholesterol, and glycemic (blood sugar) control.”
Testosterone replacement therapy for men continues to receive a great deal of medical support and, as you can see, the benefits are well documented in a multitude of clinical trials dating back as far as the1940s.
Testosterone replacement for women is equally important and for many of the same reasons. This therapy has been around since 1936, however the myths about side effects have left many afraid to try it. The truth is these rarely occur at low doses (which Hormonal Health and Wellness Centers are experts at administering).
Estrogen is a woman’s most important hormone. During her childbearing years—normally the healthiest—the ovaries produce a balance of three estrogens: estradiol, estriol and estrone. Estradiol is the predominant estrogen, created in twice the quantity of the other two. A woman’s body must maintain this ratio of two to one to function optimally. If the ratio is altered, the result is too much estrone, which is a very powerful breast stimulator. Women often complain of breast tenderness when taking oral estrogen because the ratio is disturbed resulting in too much estrone.
Estrogen receptors exist in a variety of organs throughout the body—the brain included. That’s why estrogen loss produces so many different bodily symptoms like loss of skin elasticity, bone shrinkage, mood and cognitive decline. On the other hand, when estrogen levels rise as they do in the first week of menses, their overall effect is to increase the amount of serotonin available in the spaces between the brain’s nerve cells. That improves mood. Within the brain, estrogen may in fact act as a natural antidepressant and mood stabilizer.
Research increasingly demonstrates a strong relationship between loss of estrogen and increased risk for POF (premature ovary failure), osteoporosis, heart disease, colon cancer, Alzheimer’s disease, tooth loss, impaired vision, Parkinson’s disease and diabetes. The longer a woman is without the protection of her own estrogen, the greater the risk for serious health consequences from these conditions.
Regardless of age or stage of life, every woman needs her estrogen. According to noted physician, lecturer and author, Dr. Richard Gambrell, “postmenopausal women must continue estrogen therapy in adequate dosages for many years to achieve the maximum benefits. The lowest effective dosage for the shortest period of time is invalid, as the benefits of long-term HT far exceed the risks—the WHI (Women’s Health Initiative Reports) not withstanding.”
If a woman decides to undertake hormone replacement therapy, here are some imperatives: She needs to receive estrogen that her body recognizes (bio-identical), in the proper dosage (determined by accurate testing and analysis) and delivered into the bloodstream using a method that makes hormone available around the clock—the same way the body delivers hormones.