There comes a time on our lives, and it usually sneaks up on us sooner than we expect or care to realize, in which we start feeling just a bit “off”. We’re more tired than usual, we start to gain weight without explanation (where did that belly come from!); our moods shift and we get a trifle snappy, to put it mildly. We get overly anxious, and we just don’t feel like ourselves! As the years pass, these symptoms tend to get worse, and we seek answers from our primary care practitioners; walking away more confused than ever with a hand full of prescriptions for anti depressants, anti-anxiety medications and sleeping pills! “You’re just stressed out!” we are told!
Conceivably, we may be stressed out, but have you ever thought your hormones could be wreaking all of this havoc? Well, before you start filling those prescriptions, and pop those pills, my advice is this: pay attention to your gut instinct that things aren’t quite right and do a bit of research! It may save your life….
Ah, hormones, that perplexing word we’ve become conditioned to fear. “They cause cancer!” “They cause heart attacks and strokes!” we’ve heard. How can we decipher fact from fiction? What is the difference between natural methods, prescription therapies and what is really safe and effective? Moreover, who can we trust to impart us with the correct information? Here are some answers to those questions:
What is the difference between “bio-identical” and “synthetic” hormones?
By “bio-identical” we mean that the structure of the hormone is perfectly matched to the hormone produced in a woman’s body. They are plant-based, natural substances that our bodies can metabolize in the way it was designed, minimizing side effects. These compounded bio-identicals can be matched to each woman’s unique needs, something that’s impossible with mass-manufactured products.
Synthetic hormone replacement therapies are either a horse’s hormone or an artificially formulated one that is intentionally manufactured to be slightly different from human hormone in order to patent it.
The best analogy to compare the two is to look at hormones and the receptors that they work within the body as a lock and key. The lock is the receptor on the cells that the hormones act upon, and the key is the hormone itself. The bio-identical “key” fits perfectly in the lock, therefore providing the exact use that is intended by the human body, thus reducing untoward side effects. Traditional synthetic hormone “keys” do not fit the lock well, and as a result do not provide the exact action intended. Worse, they can activate negative processes in the body that can have devastating, lifelong consequences such as stroke, breast cancer, cardiovascular disease, and others!
I want a natural alternative, but I’ve heard mixed reviews about the different methods.
Most bio-identical hormone delivery methods: creams, pills, injections and even miniscule capsules do not provide the balanced hormones that factor into good health. Creams are messy, have to be put on daily, and if you travel, what a pain! Patches are a bit better, but the absorption of any skin-based method is variable, and often we loose sensitivity over time and need to search for a new spot to rub the cream or stick the patch.
Hormone pellets on the other hand, placed under the skin, deliver a constant stream of hormones into your bloodstream twenty-four hours a day, seven days a week in a way that mimics your body’s natural release of hormone. Having been researched and developed since the 1930’s, they are also the most widely studied form of bio-identical hormone replacement therapy (HRT).
I’ve heard about estrogen and progesterone, but women need testosterone too?
Estrogen is a woman’s most important hormone. Without hormone replacement therapy, the loss of estrogen puts her at increased risk for premature ovary failure, osteoporosis, heart disease, colon cancer, Alzheimer’s disease, tooth loss, impaired vision, Parkinson’s disease and diabetes. The longer a woman is without the protection of her own estrogen, the greater the risk for serious health consequences of these conditions.
However, testosterone hormone therapy gives a woman her mental clarity, libido and muscle tone and mass. When this hormone is at low levels, women often complain of mental confusion, weight gain and poor muscle growth even with regular exercise. The effect of hormone deficiency on the brain, muscle, bone, heart and metabolism can be significant without hormone replacement therapy for women and dangerous to long-term health. The brain needs normal amounts of testosterone in balance with estrogen to produce serotonin, which supports emotional balance. When lacking in these hormones, a woman will experience emotional instability that often results in increased anxiety, irritability, sleep disturbances, anger, sadness and depression.
Why do I need these hormones? What if I’m past all that “hot flash stuff”?
Hormone fluctuation and depletion wreaks havoc in the body! Research evidence repeatedly points to the relationship between hormonal imbalance and an increased risk for developing cancer, osteoporosis, stroke, thyroid disorders, diabetes, heart disease and other age-related disease processes.
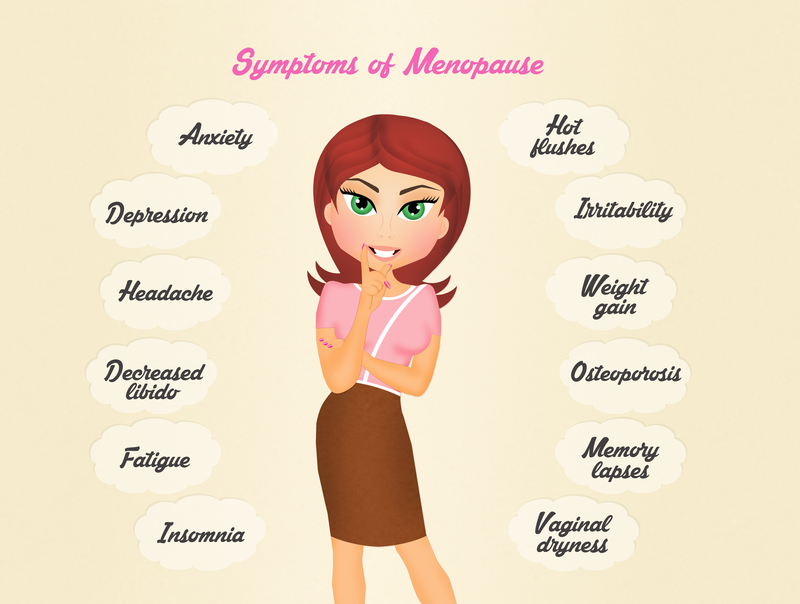
During pre-menopause, menopause and andropause (the male version of hormone depletion), it’s actually considered the norm for men and women to experience a decline in health. You’re also more likely to experience problems like depression, anxiety, memory loss, hot flashes, sleep disturbances, libido issues, and sexual dysfunction, to name just a few. Who wants to feel all of that in our “golden years”? This is not “normal” and who wants to feel “normal” for their age?
And ladies hear this: Hormone imbalance starts 10-15 YEARS before hot flashes! So don’t use that as an indicator of your hormone balance!
Again, pay attention to that little voice that is telling you “things aren’t quite right”, those inner voices are usually spot on! Most importantly, you want to find a highly trained practitioner who will not only listen to your specific fears and concerns, but who understands the intricate nature of hormone BALANCE….that is the key.
Copyright © Terri J. DeNeui 2016